What is Inflammatory Bowel Disease (IBD)?
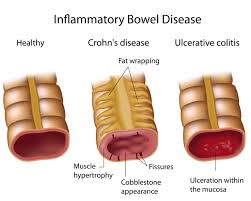
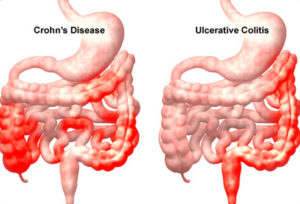
Crohn’s disease and ulcerative colitis are two forms of inflammatory bowel disease (IBD) that cause chronic inflammation of the gastrointestinal tract.
Ulcerative Colitis:
- Inflammation is limited to the colon
- Affects the innermost lining of the colon
- None of the colon is spared from inflammation
Crohn’s Disease:
- Inflammation occurs anywhere in the GI tract from the mouth to the anus
- Can affect the entire thickness of the bowel
- Inflammation is usually in patches, leaving healthy tissue in between diseased tissue
Symptoms:
- Chronic Diarrhea (or constipation)
- Rectal Bleeding
- Urgency
- Abdominal pain
- Fever
- Loss of appetite
- Fatigue
- Night sweats
- Mouth sores (Crohn’s)
In severe cases, Crohn’s disease may lead to tears (fissures) in the lining of the anus and fistulas. Fistulas are tunnels that connect one loop of intestine to another or to the skin, vagina, or bladder.
How are Crohn’s & Colitis Diagnosed?
- Colonoscopy & Upper Endoscopy with Biopsies (gold standard test; biopsies can show areas of inflammation that may not be visible to the naked eye)
- MRI & CT Scans (can show inflammation in areas the scope may not reach)
- Blood tests (shows inflammation levels, nutrient deficiencies)
(A colonoscopy sounds horrible, but I promise I have had four of them, and they are not bad at all. People say the worst part is the prep, but it is not painful like normal diarrhea. The procedure itself is simple: you get an IV, go to sleep, wake up, and then go about the rest of your day).
Who is Affected by Crohn’s & Colitis?
- Crohn’s affects 780,000 Americans
- Ulcerative colitis affects 907,000 Americans
- Men and women are equally affected
- IBD is more commonly diagnosed in adolescents and young adults between age 15 and 35
- IBD tends to run in families (hereditary)
- People of Northern European descent are more commonly affected
What Causes Crohn’s & Colitis?
While the cause of Crohn’s & Colitis is not fully understood, research shows that genetics and environmental factors contribute to their development. Crohn’s & Colitis are autoimmune diseases, meaning that the immune system falsely views the body’s healthy cells as foreign invaders and attacks, causing inflammation and ulceration. Additionally, the immune system attacks the bacteria, fungi, and viruses in the gastrointestinal tract (that’s why it is important to build up your good bacteria with prebiotics and probiotics).
What are the Treatments for Crohn’s & Colitis?
Traditional Treatments
- Aminosalicylates (5-ASA)
- Corticosteroids (prednisone, budesonide)
- Immunomodulators (6-mercaptopurine, methotrexate)
- Antibiotics (Flagyl, cipro)
- Biologic Therapies (Humira, Remicade, Cimzia, Tysabri, Stelara)
There are many potentially severe side effects associated with these medications, such as an increased risk of cancer, serious infections, and more. However, leaving the inflammation untreated is also very dangerous, as inflammation drastically raises one’s risk of developing cancer. Additionally, quality of life is really important, so the benefits of starting a medicine with potentially bad side effects may outweigh the risks.
Complementary/Alternative Medicine
Nutrition, exercise, and lifestyle are also very important in managing these chronic conditions. Many people follow anti-inflammatory diets like the Autoimmune Paleo Diet (AIP) and the Specific Carb Diet (SCD) and have been able to come off of medication completely. Healing and rebuilding the microbiome (natural microorganisms like bacteria and viruses) takes time, so it is important to keep that in mind when it seems like no medicine or diet is working. It is my goal to stay on medication for as long as I need to, then eventually control the inflammation on my own with diet.
Source: Crohn’s & Colitis Foundation of America (CCFA)